Naloxone: Is It Really a Wonder Drug?
For many New Jersey residents, June 18 was a historic day. Samantha Newton appreciated its importance. She left the house early that morning to line up for a one-time freebie. She had to do this because supplies might run out. This giveaway was not from a holiday sale or mall opening, but a matter of life and death. The queue was for naloxone, the antidote for opioid poisoning—offered free and without prescription— for one day only. Newton got one for her brother, an opioid addict in rehab, in case he relapsed.
The promotion was part of New Jersey’s drug abuse control task force initiated by former governor Christopher Christie in 2017, who was tapped to lead the presidential commission against the opioid crisis. The move was necessary because Christie found out that although civilians can get 4mg of Narcan (the nasal spray form of naloxone), not all emergency responders are permitted to use more than 2mg doses. With the rise of new, more malignant strains of opiate fentanyl, a higher naloxone dose was necessary. So he revised guidelines for the health department, allowing first responders to carry double the dosage of naloxone to reverse the potent symptoms of an opioid overdose. Christie’s successor, Phil Murphy, took over the task force when he assumed office in 2018 in the wake of 3,100 drug deaths.
The National Institute on Drug Abuse (NIDA) estimated that 300,000 people have died in the US from opioid overdose since 2001. The opioid epidemic is the main cause of death for US adults aged 50 and younger, overshadowing traffic accidents.
In 2018, US Surgeon General Jerome Adams issued a public health advisory calling on more Americans to carry naloxone. He said that making naloxone products more accessible and expanding treatment services could help manage opioid overdoses. As a result, all states passed laws to increase naloxone availability. In most states, one can buy Narcan without a prescription. New Jersey’s Camden County now supplies Narcan in all schools. US pharmacies still require people to buy it, either out of pocket or through their insurance company or Medicaid.
Fortunately, Canadians can obtain naloxone free from pharmacies through our healthcare system. This is significant because our neighbours down south have to resort to charity. More US government agencies are relying on partnerships with hospitals or donations from pharmaceuticals just to make the medication affordable.
What is it?
Naloxone hydrochloride is a semi-synthetic drug used to revive those who have suffered an opioid overdose, like heroin and opium. It belongs to the drug group ‘antidote to narcotic drug poisoning’. It helps counteract symptoms of overdose on prescription opioid medications such as Percocet (oxycodone), Avinza, Astramorph PF, Duramorph, Infumorph, Kadian, MS Contin (morphine), and Zohydro (hydrocodone).
Patients who consume high doses of opioids usually become extremely drowsy, they experience severe respiratory depression, and they lose consciousness. Naloxone revives them and helps them breathe normally again.
What are its other names?
Narcan and Evzio are brand names of the generic naloxone hydrochloride.
Who makes it?
Adapt and Bristol Myers Squibb market the brand name Narcan for the nasal spray. Kaleo manufactures the auto-injector version. Other naloxone manufacturers are Amphastar, Hospira, Mylan, and West-Ward.
How is it packaged?
Naloxone comes in different formats:
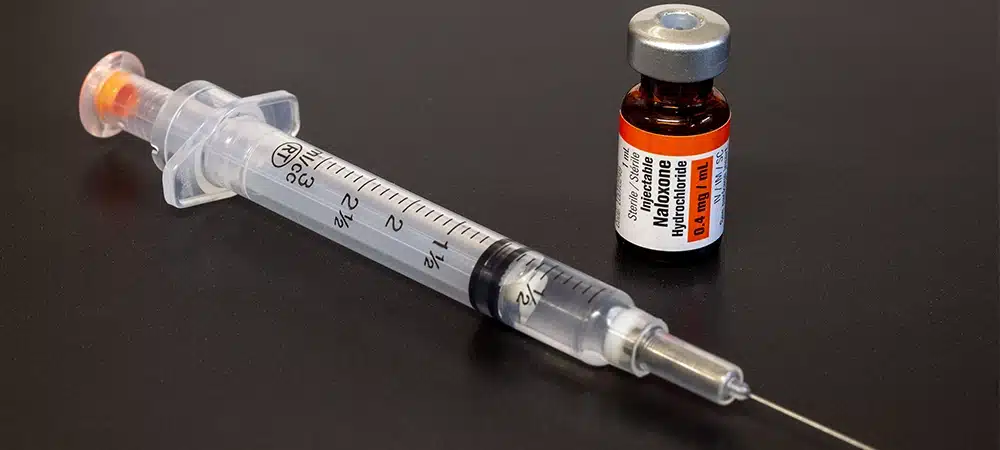
- The liquid formulation is injected into a muscle, under the skin, or into a vein through an IV. It is used by medical professionals (paramedics, ER doctors), or a family member/caregiver trained to inject medications. The FDA approved the brand Narcan in 1971. Though the branded naloxone injection has been discontinued, generics have been available since 1985. Current injections come in two doses: 0.4mg/mL and 1mg/mL.
- Evzio, the auto-injectable version, is a prepackaged device that automatically injects a measured dose into the thigh. The unit gives verbal instructions, so even a non-medical person can deliver the medication. The package comes with two doses.
- The needle-free Narcan nasal spray comes in a concentrated 4mg dose administered through the nose. It is the first and only nasal naloxone available in North America.
How does one store it?
Naloxone should be stored at room temperature (15-30℃) away from moisture and heat. Auto-injectors should be kept in their original packaging until use. Check the expiration date. If the medicine has changed colour or has particles, do not use it.
What are its other uses?
The US Food and Drug Administration (FDA) has approved naloxone to counteract life-threatening depression of the central nervous system and respiratory system. Respiratory depression (or hypoventilation) means ineffective and slow breathing, which results in low oxygen levels and high carbon dioxide levels in the blood. Central nervous system depression refers to a slowed heart rate and loss of consciousness—the result of restricted brain activity—which could lead to coma or death.
Doctors administer small doses of naloxone after surgery to counteract the effects of opioids given during the operation. The antidote is also used to increase blood pressure during septic shock.
How does it work?
Naloxone temporarily blocks opioid receptors to prevent opioids from working. As a nonscheduled, non-addictive prescription medication, it cannot be used to get high. Patients who received naloxone—especially breastfeeding or pregnant women—should report it to all healthcare providers they see in the future. Those who experience unusual side effects should report these to the FDA by calling 1-800-FDA-1088.
If an overdose victim can inform first responders about current medications and health conditions (especially if the patient is a pregnant woman or has cardiovascular disease) during emergencies, they should do so before receiving naloxone injections. It is not known if naloxone passes into breast milk or if it could harm nursing or unborn babies.
How long does it take to work?
The naloxone injection’s onset of action is two minutes if administered intravenously (IV) and five minutes if given intramuscularly (IM). The spray’s onset of effect is 30 seconds to three minutes. Naloxone stays in the system for only 30 to 90 minutes, and the effects of opioids last longer, so rescuers need to call 911 before giving it so that medical backup can arrive before the naloxone wears off.
How is the dosage timed?
Single doses are given at two- to three-minute intervals and repeated if necessary. The patient’s condition and response determine treatment duration and dosage frequency.
When is it safe to stop giving it to an overdose patient?
When erratic breathing has returned to normal, and when narcotic poisoning symptoms have resolved.
However, don’t assume that an overdose episode has ended. Emergency medical services (EMS) are still needed.
Can one overdose on it?
If the administration of naloxone (the injectable kind) is done by a trained professional, an overdose is unlikely. None has been reported for the spray. Naloxone’s overdose danger and dependence ratings are low.
Will it work for other kinds of overdose?
No, naloxone only works on the effects of opioids. It may not work well in preventing the effects of some opioid types, such as mixed agonists/antagonists like pentazocine. In this case, blocking may be incomplete, so a higher dose of naloxone may be necessary.
Negative effects of naloxone
When given to known or suspected narcotic addicts, the naloxone injection may trigger severe, but temporary withdrawal symptoms. So one should be extremely careful. More attention should be given when administering to newborns, and pregnant and nursing women. Though naloxone is unlikely to have lasting adverse effects on breastfeeding, it should only be given to an addicted mother in an emergency situation, when her life is at risk. If necessary to save the lives of infants or children, administer a reduced dose. No problems have been reported in those aged 60 and over.
This is a partial list of side effects:
- Gastrointestinal conditions: stomach cramps, nausea, vomiting, and diarrhea.
- Some patients experience mood swings, aggression and irritability.
- Naloxone may slow down reflexes and impair thinking.
- Alcohol increases naloxone’s side effects.
- Pain relievers may not work while patients are on naloxone.
- Allergic reactions include hives, flushing, difficulty breathing, and swelling of the face, lips, tongue, or throat. On or near the injection site, pain, burning, or redness can occur.
- As naloxone reverses the effects of opioids, it may cause sudden withdrawal symptoms such as gastric and cardiac problems, respiratory depression, fever, body aches, weakness, anxiety, restlessness, shivering, watery eyes, sneezing, and runny nose. In infants younger than four weeks, stiffness, seizures, and overactive reflexes can occur.
- Rebound opioid toxicity may come after naloxone treatment. The rebound effect (or rebound phenomenon) is the reappearance of symptoms after the medication is discontinued, worn off, or reduced in dosage. Symptoms are often worse than before.
- In rare cases, these occurred: increased sweating, convulsions, seizures, cardiac arrest (the heart stops beating), tachycardia (abnormally fast heart rate), and ventricular fibrillation (irregular heart rhythm). Palpitations happened only in very sick people treated with multiple doses.
- After surgery, these have occurred: hypotension (abnormally low blood pressure), hypertension (abnormally high blood pressure), dyspnea (laboured breathing), pulmonary edema (fluid in the lungs), encephalopathy (brain function abnormality), coma, and death.
Where can one obtain the spray?
In the US, most major insurance plans cover Narcan nasal spray. In recent years, major pharmacies (CVS, Walgreen, RiteAid) have been selling it without a prescription.
In Canada, the National Association of Pharmacy Regulatory Authorities (NAPRA) classified Narcan for emergency opioid overdose use as a Schedule II drug in December 2016. So patients can obtain it from a community pharmacist without a prescriber’s note.
Narcan is free for Non-Insured Health Benefits (NIHB) Program clients across Canada. It is also available free from Ontario and Québec pharmacies. In British Columbia, Alberta, and Saskatchewan, it is an unscheduled drug, so it can be purchased outside of pharmacies.
Profiteering
A 2016 research published by Gupta et al in the New England Journal of Medicine found naloxone manufacturers profiting off naloxone. Amphastar, Hospira, and Kaleo increased prices by 95-500% from inception year to 2016. Mylan, West-Ward, and Adapt kept prices the same. Although shocking, Gupta said it was part of an overall trend of increasing prescription drug prices, both generic and branded. One negative impact? First responders in certain areas are already scrimping on naloxone, deploying one dose instead of two. If prices go unchecked, there will come a time when the cost becomes so prohibitive that very few can afford it, leading to more drug deaths.
Combination antidotes
Naloxone, as an opioid antagonist, has been combined with other therapies to curtail opioid use disorder. It has been added to buprenorphine to create suboxone. Naloxone prevents the user from getting high from buprenorphine. Suboxone’s rival is naltrexone. Both suboxone and naltrexone are effective in treating addiction to heroin and prescription painkillers and managing alcohol or opioid dependence.
What’s the difference between naltrexone and suboxone?
Though naltrexone and suboxone both curb opioid cravings, they differ. Sold under the brand names ReVia and Vivitrol, naltrexone (administered orally or by injection) should be given to patients only after they’ve completed detox. The injection is administered only once a month. Suboxone is a daily oral medication that can be used before or after detox.
Instructions for use
Narcan Spray
This is for nasal use only. A non-healthcare professional can administer it before emergency medical help becomes available, but it is not meant to be a substitute for professional medical care. Before giving naloxone, rescuers should call 911 first.
- Check for signs of an opioid overdose:
- The patient does not wake up even after you shake them, shout at them, or firmly rub the middle of the chest.
- The patient is experiencing respiratory depression or slow, irregular breathing.
- Pupils usually resemble a pinpoint.
- Lay the person on their back.
- Take the spray out of its packaging. Do not test it because there is only one dose per device.
- Tilt the patient’s head back and support his neck with your hand.
- Hold the device with your thumb on the plunger’s base. Put your first and middle fingers on either side of the nozzle. Gently insert the tip of the nozzle into one nostril. For children, the nozzle should seal the nostril. Press the plunger firmly with your thumb to give the dose. Alternate nostrils with each dose.
- Move the person to the recovery (side) position. Watch them closely.
- If shallow breathing persists or stops, continue rescue breathing while waiting for naloxone to take effect.
- If the person has not woken up, or their breathing has not improved, give a second dose after 2-3 minutes.
- If the second dose of naloxone doesn’t work—the patient isn’t responding to stimulation, is not breathing, and has no pulse—the heart has already stopped, opioids are not in their system, or the opioids are really strong (especially fentanyl). So give more naloxone or perform cardiopulmonary resuscitation (CPR).
Injectable naloxone
This comes in two forms: a multi-dose 10mL vial and a single-dose 1mL flip-top vial. Follow the steps above for recognition of, and response to, an overdose. Then inject the naloxone as follows:
- If the person is not breathing, perform artificial respiration for a few quick breaths.
- Use a long 1 to 1.5-inch intramuscular needle (IM) from pharmacies or needle exchange programs.
- Flip the orange top vial. Draw up 1cc (1mL or 100u) of naloxone into the syringe.
- Inject straight into a muscle: the outer thigh, the upper and outer quadrant of the buttocks, or the shoulder. If a long needle isn’t available, a shorter one can be used to inject under the skin. During emergencies, one can inject through clothing. Each Evzio auto-injector is for one use only. Discard leftovers.
- After injection, continue rescue breathing for 2-3 minutes. If there’s no change, administer another dose of naloxone and continue rescue breathing.
- If the second dose of naloxone doesn’t revive the patient, see the last instruction paragraph for the atomizer.
Naloxone revives not just the patient, but also opioid withdrawal symptoms, causing him to want to dope again. This may lead to another overdose, so rescuers should stay with the patient should he need more naloxone, and to keep him from retaking opioids.
Fighting naloxone’s stigma
Dr. Joan Papp started MetroHealth’s ProjectDawn Initiative in 2013. ProjectDawn makes naloxone kits available to the public at the scene of an overdose. Now, even police officers are trained to administer the drug. MetroHealth’s Peer Supporter program connects people in recovery or ‘peer supporters’ licensed by the state to work with ER patients with substance use disorders.
Dr. Papp comments on the stigma surrounding naloxone: “There was a lot of pushback in the beginning because of the belief that we were enabling drug use or supporting it in some way. But as more people become familiar with the program, and they see the benefits of having naloxone available, and its lifesaving effects, attitudes have shifted. We’re seeing a lot more support now. As awareness of the epidemic has grown, folks understand this is something that affects not just strangers, but people they know as well.”
Proven effectiveness
As with similar medications like naltrexone, naloxone is leading the fight against the opioid overdose problem. If there is an addict in the family or a recovering one in danger of relapsing, having naloxone handy is mandatory. All caregivers and members of the household should know how to use it.
With naloxone manufacturers continuing to increase prices, hopefully, other cheaper, more accessible competitive antagonists will surface soon. Of course, there’s always the option of quitting opioid abuse. But that is easier said than done.