What Are Benzodiazepines (Benzos)?
Benzodiazepines, often called “benzos”, are a class of central nervous system depressants that reduce brain activity by enhancing the effect of the neurotransmitter GABA. This action produces calming, sedative, and muscle-relaxing effects. They are mainly prescribed for short-term treatment of conditions such as anxiety disorders, panic attacks, insomnia, seizures, and sometimes muscle spasms. Common examples include Valium (diazepam), Xanax (alprazolam), and Klonopin (clonazepam).
How Benzodiazepines Work
So, how do benzos work exactly? At the simplest level, they help slow things down in the brain. They boost the activity of something called GABA—that’s a neurotransmitter, a chemical that helps calm nerve activity. Think of GABA like the brain’s built-in brake system. When it’s working well, it helps keep your thoughts and reactions from spinning out too fast.
Benzos basically amplify that calming signal. So if your brain is racing, if anxiety is making everything feel out of control, a benzo can feel like someone turned the volume way down. Not off, just… quieter.
And that’s a big reason why people find them so helpful. For someone having a panic attack, the relief can come in under an hour. It can feel like finally getting your head above water after thrashing around in a storm. I’ve heard some people describe it as a kind of emotional silence—just stillness, finally.
But here’s where it gets tricky. That calm? That fast-acting relief? It can also make benzos something people rely on a little too much. Not because they want to, necessarily. It just sort of happens over time.
Why Benzodiazepines Are Prescribed
Doctors prescribe benzos for a few different reasons. Anxiety is the big one. Not just day-to-day worry, but full-on, overwhelming anxiety that can stop people in their tracks. Panic attacks. Nighttime anxiety that keeps you from sleeping. Or chronic tension that never quite lets go.
They’re also used for:
- Insomnia
- Seizures or epilepsy
- Muscle spasms (like after a spinal injury)
- Alcohol withdrawal
- Pre-surgery nervousness
Used short-term, and under the right conditions, they can be incredibly effective. But even when used exactly as prescribed, there’s still a chance of running into problems—tolerance, dependence, withdrawal. Things most people aren’t warned about until they’re already feeling the effects.Suggested Table: Common Benzodiazepines and What They’re Usually Prescribed For
|
Medication |
Also Known As |
Common Use |
How Long It Lasts |
|---|---|---|---|
|
Alprazolam |
Xanax |
Anxiety, panic |
Short |
|
Diazepam |
Valium |
Muscle spasms, anxiety |
Long |
|
Lorazepam |
Ativan |
Anxiety, calming before surgery |
Medium |
|
Clonazepam |
Klonopin |
Seizures, chronic anxiety |
Long |
|
Temazepam |
Restoril |
Sleep problems (insomnia) |
Medium |
Are Benzodiazepines Addictive?
This is where the conversation around benzodiazepines tends to get a little heavier. Yes, benzodiazepines can be addictive. But the word “addictive” can mean different things to different people, so maybe it’s worth unpacking a bit.
You don’t have to abuse benzos to develop a problem. That’s a common misunderstanding. Even people who take them exactly as prescribed can find themselves struggling with dependence. It can happen gradually, often without realizing it. Maybe your usual dose doesn’t seem to work as well anymore. Or maybe you start feeling uncomfortable—restless, irritable, even shaky—when you miss a dose or try to taper off.
That’s not weakness or misuse. It’s biology.
Tolerance and Physical Dependence
The brain adapts quickly. The more often you use benzodiazepines, the more your brain starts to expect that extra GABA activity. Over time, it can stop producing as much of its own calming chemicals, because it assumes you’ll supply them from the outside.
This is what leads to tolerance—needing more of the drug to get the same effect. And eventually, it can turn into physical dependence. That doesn’t mean addiction in the way people often imagine it, with cravings or compulsive behavior. But it does mean your body has come to rely on the medication to function “normally.”
I remember reading a story about someone who was prescribed Ativan after a traumatic event. She took it once a day for a couple of months. Nothing extreme. But when she tried to stop, she felt like her nervous system was falling apart. Her heart would race. Sleep became nearly impossible. She was never warned that something like that could happen.
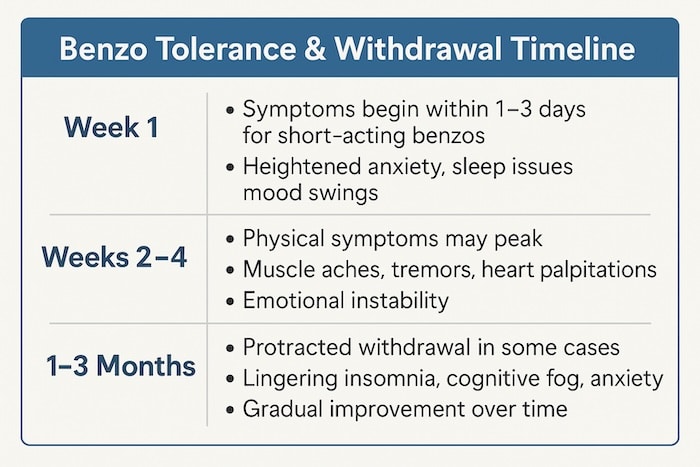
What Withdrawal Feels Like
Benzodiazepine withdrawal can be intense—and in some cases, even dangerous. Symptoms can range from mildly uncomfortable to deeply distressing. They might include:
- Anxiety (often worse than before)
- Insomnia
- Muscle tension
- Tremors
- Sweating
- Nausea
- Heart palpitations
- In rare cases: seizures
What’s frustrating is that withdrawal symptoms can sometimes be mistaken for a return of the original condition. Someone trying to stop their medication might think their anxiety is coming back, when really, it’s their body reacting to the sudden absence of the drug.
This is why doctors usually recommend tapering slowly, over weeks or even months, depending on how long you’ve been taking the medication and at what dose. Quitting “cold turkey” is generally not safe, especially with long-term use.
Are All Benzos Equally Risky?
Not exactly. Some benzodiazepines have a shorter half-life, meaning they wear off faster. These tend to cause stronger withdrawal symptoms. Others stick around in your system longer, which can make the transition off of them a little smoother—but not always.
It’s complicated, honestly. And very personal. What feels manageable for one person might feel overwhelming for another. There’s no one-size-fits-all approach here, which is part of what makes treating benzo dependence so challenging.
What Are the Side Effects of Benzodiazepines?
Most people who’ve taken benzodiazepines—especially early on—will tell you they work. And they do. The calm is real. The relief is often fast. But that doesn’t mean the experience is always smooth. Even short-term use can come with some side effects, and long-term use can add a whole new layer of complications.
Common Side Effects
At first, side effects might be subtle. You might feel a bit groggy or slow. Some people describe it as a kind of brain fog, like their thoughts are moving through molasses. Others feel sleepy during the day or a little off-balance. Not bad enough to stop entirely, maybe, but enough to notice.
Some of the more common short-term side effects include:
- Drowsiness
- Dizziness or lightheadedness
- Confusion
- Blurred vision
- Nausea
- Slurred speech
- Coordination issues
It’s the kind of thing that might make you pause before driving or using heavy machinery (and yes, doctors will usually advise against both). If you’re older, these effects can be more pronounced and even risky. A simple fall, caused by slightly slower reflexes, can lead to serious injury.
Memory and Thinking Problems
One of the more concerning side effects of benzodiazepines, especially with regular use, is the impact on memory. People sometimes report forgetfulness, trouble concentrating, or just feeling mentally dull. Not everyone experiences it, but when it happens, it’s hard to ignore.
There’s even a term—“benzo brain.” It’s not medical, but it comes up a lot in support groups and forums. People describe it as living in a fog, being present but not fully engaged. Like they’re watching their life from a few steps behind.
Some studies suggest that long-term benzo use may increase the risk of cognitive decline, especially in older adults. There’s even been talk about a potential link to dementia, though the research is still ongoing and a bit murky.
Emotional Blunting and Disconnection
Here’s something that doesn’t show up in prescription pamphlets: for some, benzodiazepines don’t just dull anxiety—they dull everything. That includes joy, curiosity, motivation. It’s as if the emotional volume gets turned down across the board.
Someone might feel less anxious but also less alive. Less connected. It’s subtle, and maybe not everyone notices it right away. But for those who do, it can feel like losing part of yourself.
That emotional flattening can have ripple effects, too—on relationships, on work, on creativity. Again, not universal. But real enough that it’s worth mentioning.
Long-Term Risks
If used occasionally and in small doses, many of these issues are minor or temporary. But with long-term or frequent use, risks start to grow. These might include:
- Physical and psychological dependence
- Cognitive decline
- Worsening anxiety or depression (ironically, after withdrawal)
- Reduced coordination and increased fall risk
- Difficulty tapering off
The tricky part is that benzodiazepines are often prescribed during emotionally intense times—grief, trauma, panic. In those moments, long-term risks may not even cross your mind. And sometimes, the prescriber doesn’t bring them up either.
That’s not to say benzos are “bad.” But they come with a weight, a cost, that isn’t always obvious at the start.
“Short-Term vs. Long-Term Side Effects of Benzodiazepines”
|
Effect |
Short-Term Use |
Long-Term Use |
|---|---|---|
|
Drowsiness |
Common, usually mild |
Persistent, worsens with age |
|
Memory issues |
Rare |
Moderate to severe |
|
Coordination problems |
Possible |
Increased fall risk |
|
Emotional numbing |
Uncommon |
More likely over time |
|
Dependency/withdrawal risk |
Low |
High |
Can You Take Benzodiazepines Safely?
The short answer? Yes, benzodiazepines can be taken safely. But—like a lot of medications that affect the brain—it really depends on how they’re used, for how long, and under what circumstances.
That’s not meant to be vague. It’s just that “safe” isn’t always a fixed thing. What’s safe for one person might not be for another. A single dose before a dental procedure? Probably fine. Taking a small daily dose for five years without any changes or re-evaluations? That’s… a little murkier.
When They Make Sense
There are situations where benzos genuinely make a lot of sense. If someone is experiencing an acute panic attack that isn’t responding to other interventions, a fast-acting benzo like alprazolam (Xanax) can bring relief within minutes. That can be a lifesaver—literally.
Same goes for things like:
- Seizure management, especially when rapid control is needed
- Alcohol withdrawal, where benzos can help prevent dangerous complications like seizures or delirium
- Short-term anxiety, like before a surgery or MRI, where other treatments aren’t practical
In those contexts, short-term, carefully monitored use is both effective and appropriate. Most side effects are manageable, and the risk of long-term issues is low.
What “Safe Use” Actually Looks Like
Here’s what safe use of benzodiazepines usually involves:
- Lowest effective dose: The goal isn’t to numb every anxious thought, just to get things under control when needed.
- Shortest possible duration: Often this means a few days to a few weeks, not months or years.
- Intermittent, not daily: Using benzos only when truly needed, instead of every day, reduces the risk of tolerance and dependence.
- Frequent reassessment: Your doctor should check in regularly, making sure the medication is still necessary and working as intended.
- Avoiding alcohol and other sedatives: Combining substances that depress the nervous system can be risky—even fatal in some cases.
It’s not always easy to stick to these guidelines. Life is messy, and mental health is complicated. Sometimes a short-term prescription becomes long-term out of necessity. Sometimes no other treatment has worked. That doesn’t make anyone a failure. But it does make honest conversations more important.
The Importance of Supervision
Benzodiazepines shouldn’t be a solo journey. If you’re taking them, even occasionally, it’s worth having an open, ongoing dialogue with your doctor or psychiatrist. Let them know how you’re feeling. If you’ve noticed changes in mood or memory, say so. If you’re starting to feel like you need the medication just to get through a regular day, that’s important to bring up.
There’s still a bit of stigma around dependence—around needing help tapering off or switching to a different treatment. But the truth is, many people need help at some point. That’s not a weakness. That’s just… being human.
Alternatives to Benzodiazepines
Sometimes, the question isn’t whether benzodiazepines work—it’s whether something else might work just enough without the long-term risks. And to be fair, there are alternatives. Some are medical, some therapeutic, and some fall more into the lifestyle and daily habits category. None of them are quite as fast or dramatic as a benzo, but they also don’t come with the same potential for dependence or withdrawal.
That trade-off, honestly, is where most people struggle.
Other Medications
Let’s start with the most direct substitutes: other prescription medications that treat anxiety, sleep issues, or muscle tension.
- SSRIs and SNRIs (like sertraline, escitalopram, or venlafaxine) are often first-line treatments for anxiety and depression. They don’t work instantly—in fact, it can take weeks to feel a shift—but they’re much safer for long-term use.
- Buspirone is a lesser-known anti-anxiety medication. It works differently than benzos and doesn’t carry the same risks of sedation or dependence. It doesn’t work for everyone, but for some, it’s a steady, non-addictive option.
- Beta blockers (like propranolol) don’t treat anxiety itself, but they do help manage physical symptoms like a racing heart or shaky hands, especially in performance situations.
- For sleep, melatonin, trazodone, or low-dose doxepin can sometimes offer a gentler approach than a sedative-hypnotic.
That said, these medications all have their own set of side effects, interactions, and pros and cons. There’s no magic pill—just different options that may fit better depending on your situation.
Therapy and Counseling
This part can sound boring or slow, especially if you’re in the middle of a crisis. But cognitive behavioral therapy (CBT), especially for anxiety or insomnia, has strong evidence behind it. Not theoretical studies or feel-good stories—actual data.
CBT teaches you how to change patterns of thought and behavior that feed anxiety or sleeplessness. It’s not about “thinking positive.” It’s more like learning how to interrupt a loop your brain keeps getting stuck in.
Other approaches—like exposure therapy (for phobias and panic), EMDR (for trauma), or even acceptance and commitment therapy (ACT)—can be incredibly helpful too. Sometimes therapy can feel frustrating or even triggering at first. That’s normal. The point is, change tends to happen slowly, and it’s not always comfortable. But the benefits tend to last.
Lifestyle and Daily Tools
Now, let’s be honest. If someone’s drowning in panic or insomnia, telling them to “just try yoga” can feel dismissive. But over time, these things do matter. They just take longer to feel the payoff.
Here are a few things that genuinely help many people manage symptoms:
- Regular exercise, especially cardio, can significantly reduce baseline anxiety
- Mindfulness or meditation, even for just a few minutes a day
- Sleep hygiene, like consistent wake times, cool dark rooms, and no screens before bed
- Caffeine reduction (not fun, but often worth it)
- Support groups, whether online or in person
None of these are quick fixes. But they can form the foundation of something more stable—especially when paired with professional support.
Benzodiazepines vs. Alternatives
|
Treatment Type |
Onset of Action |
Risk of Dependence |
Long-Term Benefit |
|---|---|---|---|
|
Benzodiazepines |
Fast (30–60 min) |
High |
Low to moderate |
|
SSRIs/SNRIs |
Slow (2–6 weeks) |
Low |
High |
|
Buspirone |
Moderate (1–2 weeks) |
Very low |
Moderate to high |
|
CBT |
Slow (weekly) |
None |
High |
|
Exercise/Meditation |
Gradual (weeks) |
None |
High |
How to Taper Off Benzodiazepines Safely
Deciding to stop taking benzodiazepines is a deeply personal choice—and honestly, it can feel a little overwhelming. There’s fear, uncertainty, and sometimes guilt wrapped up in the decision. And that’s before you even take the first step. But if you’re thinking about it, it usually means something inside you is ready for change. And that matters.
The good news? It can be done. The not-so-good news? It usually takes time, support, and patience. Probably more of all three than you might expect.
Why Tapering Is Essential
Unlike some medications that you can stop cold turkey, benzos require a gradual tapering process—especially if you’ve been using them regularly for more than a few weeks. Stopping suddenly can lead to withdrawal symptoms that range from uncomfortable to dangerous. Seizures, in particular, are a real risk with abrupt discontinuation, especially with higher doses or long-term use.
But tapering helps ease the nervous system out of its dependence. It gives your brain time to adjust, to start producing GABA on its own again, slowly.
What a Typical Taper Looks Like
There’s no universal taper schedule. Some people reduce their dose by 10% every one to two weeks. Others go even slower. And that’s okay.
Here’s a rough idea of what a taper might involve:
- Switching to a longer-acting benzo: If you’re on a short-acting one like Xanax, your doctor might switch you to diazepam (Valium). This helps avoid sudden spikes and crashes.
- Dose reduction in stages: For example, cutting down by 5–10% every 1–2 weeks. Slower if symptoms become intense.
- Stabilization periods: You don’t have to keep reducing without breaks. If things get rough, you pause. Let your body catch up.
- Ongoing monitoring: Ideally, this is done with the support of a doctor, psychiatrist, or tapering specialist.
Some people taper off in a few months. Others take a year or more. There’s no “too slow” if it keeps you safe and functional.
What to Expect Emotionally and Physically
Let’s be honest: tapering isn’t just about cutting pills. It affects your whole system—mind, body, mood.
You might feel:
- Waves of anxiety (sometimes stronger than you expected)
- Sleep disruptions
- Mood swings
- Sensory sensitivity
- Muscle tension
- A strange kind of emotional rawness, like everything is turned up a few notches
But you might also notice moments of clarity, like waking up in your own skin again. Little signs that your body is re-learning how to regulate itself. Those moments can be powerful reminders that healing is possible.
Support Really, Really Helps
You don’t have to do this alone. There are online forums (like BenzoBuddies), therapists who specialize in tapering, and even clinics in some areas that provide structured support. Having someone to talk to—even just a friend who listens without judgment—can make a huge difference.
And if you’re not ready to taper yet? That’s okay too. Just gathering information is a step. Sometimes, just knowing there’s a path out can be enough for now.
The Bigger Picture: What We’re Learning About Benzodiazepines Now
For a long time, benzodiazepines were considered a relatively safe solution for anxiety and insomnia—especially compared to older drugs like barbiturates, which had a much higher risk of overdose. Doctors felt more comfortable prescribing them, patients felt better quickly, and everything seemed… well, manageable.
But as the years have gone by, the conversation around benzos has started to shift. Slowly at first, then more urgently.
A Growing Awareness
We’re learning that while benzodiazepines absolutely have a place in modern medicine, they’re not as low-risk as once believed. Especially not when used long-term.
Studies in the last decade have linked extended benzo use with cognitive decline, increased fall risk in older adults, dependence, and in some cases, a heightened risk of developing dementia—though that connection is still debated.
And yet, many people have been on them for years, sometimes decades, with little oversight. Not because of negligence necessarily, but because tapering off these meds isn’t easy, and in many cases, there just weren’t better alternatives available at the time.
Changing Prescribing Guidelines
Medical organizations around the world are starting to respond. In recent years, guidelines from bodies like the American Geriatrics Society and the Centers for Disease Control and Prevention (CDC) have urged doctors to prescribe benzodiazepines with far more caution—particularly in older adults.
Some changes include:
- Avoiding long-term prescriptions (ideally limiting use to 2–4 weeks)
- Encouraging shared decision-making with patients
- Promoting non-drug interventions as first-line treatment for anxiety and insomnia
- Regularly reviewing ongoing prescriptions and re-evaluating risk
This shift isn’t about blaming doctors or shaming patients. It’s about learning from lived experiences—and those have taught us a lot.
What People Are Saying Matters
One of the most powerful forces behind this change hasn’t been just data or guidelines. It’s been people. Patients who’ve shared their tapering stories online. People who were never warned about withdrawal. Individuals who describe years of feeling emotionally flat or cognitively foggy—and not understanding why until much later.
These voices are pushing the medical system to be more transparent, more thoughtful, and more careful about the long-term use of psychiatric medications. It’s not about fear. It’s about respect—for the complexity of the brain, for the vulnerability of the nervous system, and for the real effort it takes to come off these drugs once you’re on them.
A More Balanced Future?
The hope is that the future of benzodiazepine use will look a little more balanced. That they’ll still be available when needed—because they are helpful—but used with more intentionality. That tapering protocols will be better understood. That doctors will have more time and resources to walk patients through safer alternatives or support them through withdrawal, when that time comes.
And maybe most of all, that we stop framing anxiety and emotional pain as something that always needs to be eliminated. Sometimes, what we need isn’t to silence the alarm, but to figure out why it’s going off in the first place.
Conclusion — So, Where Does This Leave Us?
Benzodiazepines aren’t good or bad. They’re just… powerful. And like anything powerful, they come with real benefits and real risks. That’s the thread that runs through all of this. Relief and danger, help and harm, often sitting side by side.
If you’ve taken benzos and found them helpful, that’s valid. You’re not doing anything wrong. If you’ve struggled to come off them or wish someone had warned you earlier—well, that’s valid too. These experiences don’t cancel each other out. They just paint a fuller picture of what benzodiazepines really are: complex tools that require thoughtful use.
The Value of Informed Choice
More than anything, what people seem to want is informed choice. To understand what they’re taking, what to expect, what the trade-offs might be—not five years later, but at the beginning. That kind of transparency builds trust. It also helps patients feel more in control of their own care, which, let’s face it, is half the battle.
Sometimes the right call is to take the medication, even knowing the risks. Sometimes the right move is to taper off slowly, or look for alternatives, or take a break and reassess. What matters is that the decision is made with eyes open, not out of desperation or misinformation.
Healing Isn’t Linear
If you’re someone in the middle of a benzo taper—or thinking about starting one—it’s okay if it doesn’t go perfectly. Most of the time, it won’t. You might pause. You might go backwards. You might need to stay at a certain dose longer than you expected. That’s not failure. That’s what healing often looks like: messy, slow, and hard to measure.
And if you’re not ready yet? That’s okay too. Just asking the questions and learning what’s possible is already a form of progress.
A Final Thought
There’s a quiet kind of strength in facing something as tangled as this. Whether you’re navigating anxiety without meds, tapering slowly, or just trying to understand what benzodiazepines do to the mind and body—it takes effort. It takes honesty. And it takes more resilience than most people give themselves credit for.
This isn’t about shaming medication or glorifying suffering. It’s about recognizing the full picture so people can make choices that align with their lives, not just their symptoms.
Maybe we’ll never have perfect answers. But maybe that’s okay. What we can have is better conversations, deeper empathy, and a system that meets people where they actually are—not just where the guidelines think they should be.